- Home
- Products
- Pathway
- Support
- Contact Us

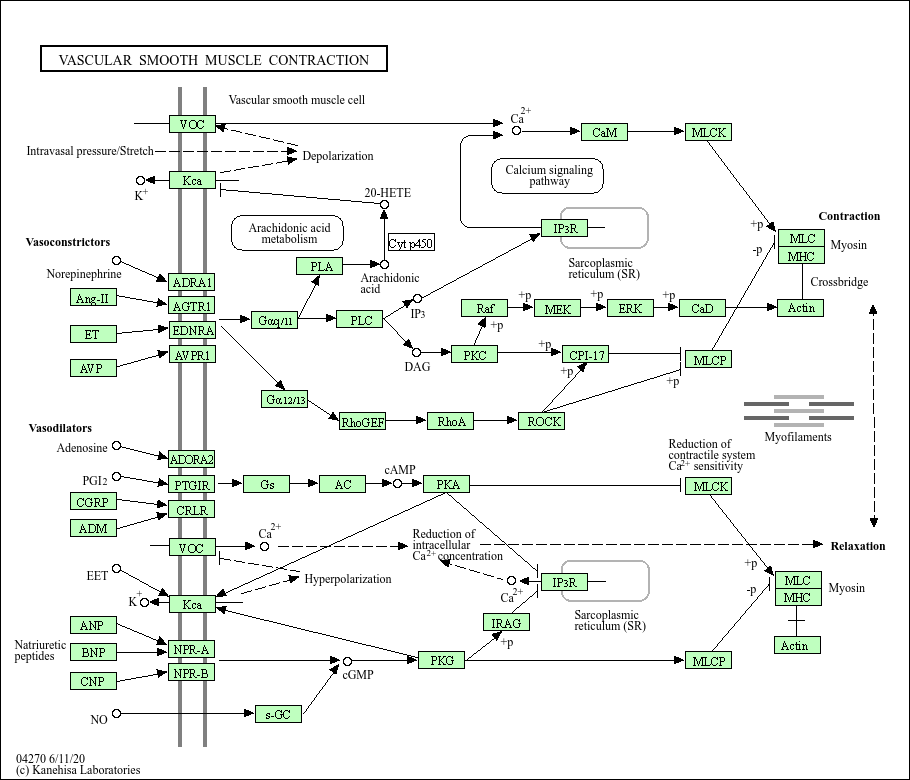
Vascular smooth muscle contraction
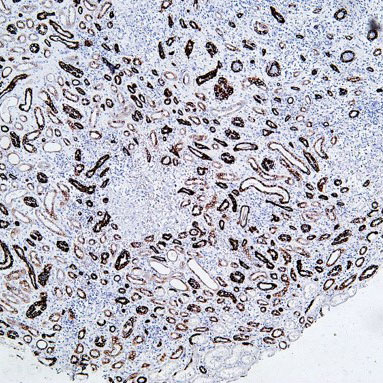
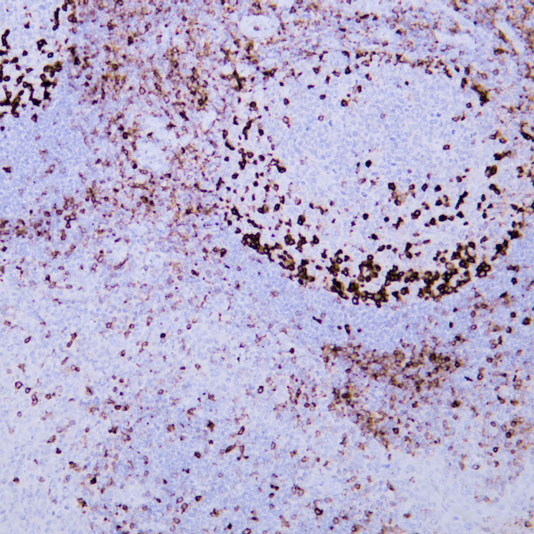
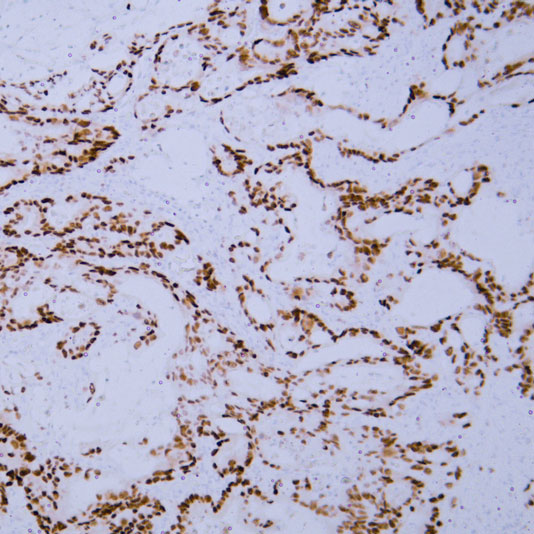
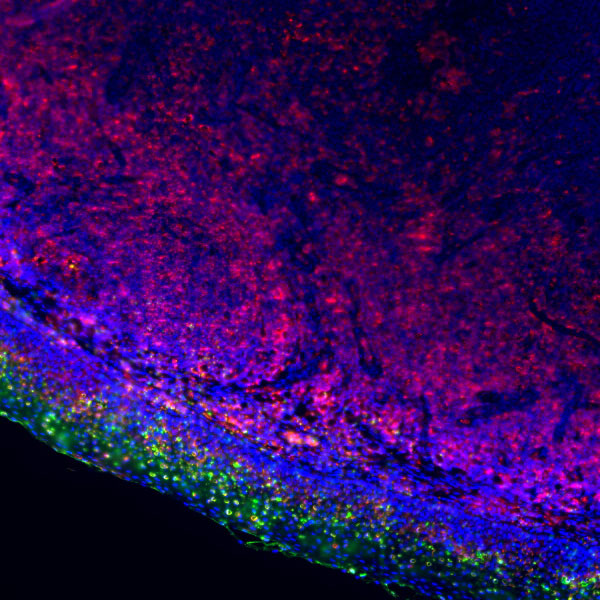
Core of basic research: Deciphers the contraction and relaxation mechanisms of vascular smooth muscle cells (VSMC) regulated by neural and humoral signals, key for maintaining vascular tone and blood pressure homeostasis. Contractile signals (e.g., NE, Ang II) bind to VSMC surface receptors, activating Gq proteins to promote PLC-γ hydrolysis of PIP2 into IP3 and DAG. IP3 induces SR calcium release, and DAG activates PKC, increasing cytoplasmic calcium concentration. Calcium binds to CaM to form a complex, activating myosin light chain kinase (MLCK). MLCK phosphorylates myosin light chains (MLC), enabling myosin heads to bind actin and trigger myofilament sliding, resulting in VSMC contraction. Relaxation signals (e.g., NO, prostaglandins) activate cGMP or cAMP pathways to inhibit MLCK activity or activate myosin light chain phosphatase (MLCP), promoting MLC dephosphorylation and VSMC relaxation. Additionally, the Rho kinase pathway enhances calcium sensitivity by inhibiting MLCP activity to regulate contraction strength. Research focuses on calcium sensitivity regulatory mechanisms, the role of the RhoA/Rho kinase pathway, the impact of VSMC phenotypic switching (contractile vs. synthetic) on contractile function, and pathway abnormalities in vasospasm, hypertension, and atherosclerosis.
Core key proteins: Vascular smooth muscle cells (VSMC), actin, myosin, myosin light chain (MLC), MLCK (myosin light chain kinase), MLCP (myosin light chain phosphatase), CaM (calmodulin), Gq protein, PLC-γ (phospholipase C-γ), IP3R (SR calcium channel), PKC (protein kinase C), RhoA/Rho kinase (regulating calcium sensitivity), NO (nitric oxide, relaxation signal), cGMP, PKG (cGMP-dependent protein kinase), Ang II (angiotensin II, contractile signal), norepinephrine (NE, contractile signal).
Core key proteins: Vascular smooth muscle cells (VSMC), actin, myosin, myosin light chain (MLC), MLCK (myosin light chain kinase), MLCP (myosin light chain phosphatase), CaM (calmodulin), Gq protein, PLC-γ (phospholipase C-γ), IP3R (SR calcium channel), PKC (protein kinase C), RhoA/Rho kinase (regulating calcium sensitivity), NO (nitric oxide, relaxation signal), cGMP, PKG (cGMP-dependent protein kinase), Ang II (angiotensin II, contractile signal), norepinephrine (NE, contractile signal).
Product list
-
{{item.title}}{{item.react}}{{item.applicat}}
Product list
Product name
Reactivity
Application
Related Resource Links
Related Promotional Journal Downloads

Explore Our Recommended Popular Products
More products
30,000+ high- quality products available online
Primary Antibodies, Secondary Antibodies, mIHC Kits, ELISA Kits, Proteins, Molecular Biology Products,Cell Lines,Reagents ...
Contact Us